Why am I at risk of OHS?
You have been considered at risk of either developing Ovarian Hyperstimulation Syndrome (OHS) or have already started to develop the syndrome, either because of the results of your treatment scans showing an excessive response of your ovaries to stimulation or because you have produced an excessive number of eggs at egg collection.
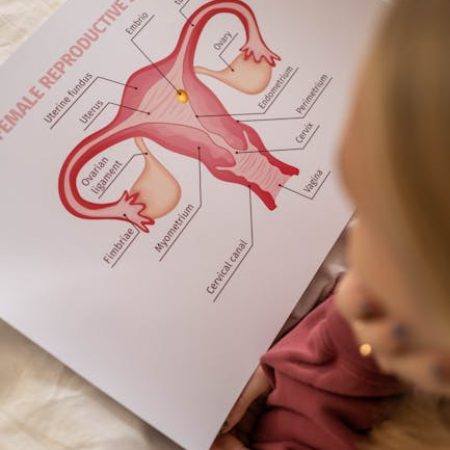
What is OHS?
OHS is a condition that is a known risk of fertility treatment and occurs when clinicians stimulate the ovaries with medication to create more than one egg. This is usually caused by injections of the hormone that stimulates your ovary.
The aim of ovarian stimulation is to produce ideally around 10-15 eggs as this is associated with an increased chance of developing good quality embryos for treatment and potential storage. Unfortunately, the responses of patients can be quite varied and unpredictable in spite of pre-treatment blood tests, and even in patients who have undergone treatment previously, and so occasionally in spite of our best attempts patients may produce an excessive response to stimulation.
Why have I over responded?
The simple answer is that you have been over-treated with the medication to stimulate your ovaries. As stated previously your clinician will ideally base your treatment regimen and dose of medication on any previous results of ovarian stimulation. For patients undergoing treatment for the first time we will utilise the results of your blood tests (particularly your AMH), age and scans. Even when utilising these results, patients may not respond as predicted, this is especially true if you are known to suffer with a condition known as Polycystic Ovarian Syndrome. In many cases, the amount of drug that is required is very difficult to assess as only very slight changes in dosage can mean the ovaries either don’t respond at all or overstimulate. For some patients it is almost impossible to get a normal response however carefully this stimulation is given.
What are the symptoms
The major symptoms are off a feeling of bloating or abdominal distension, however most patients with a successful response will have some of these symptoms. For any patients with pain or shortness of breath it is important that they are seen immediately. For many patients, because of the stimulation regimen that we use, the first signs of possible overstimulation are at your scans or on the day of egg collection when more than 20 follicles may develop.
What are the risks?
The risks of OHS can be severe, with fluid collecting within the abdominal cavity as well as dehydration that can rarely lead to blood clots. Occasionally fluid may collect in the chest cavity causing shortness of breath.
What can be done to reduce or prevent any risk?
We are pleased to say that because of the type of treatment regimen and medication that we use in addition to the drugs that stimulate your ovaries, the risk of OHS has been greatly reduced. By avoiding ovulation trigger and cancelling your egg collection, OHS can be completely avoided as a serious complication. However for most patients for whom the clinician feels are developing OHS at the time of your last scan a different trigger injection (Buserelin) can be given and all the subsequent embryos created can be frozen to be used in a subsequent cycle. This treatment, known as a ‘freeze-all’ cycle, will still remove almost all the risk and symptoms of OHS whilst still allowing your eggs to be collected.
For the occasional patient who becomes more symptomatic in spite of our modern treatment, admission to the ward, fluids given intravenously as well as injections to thin your blood and daily blood tests may be required.
Won’t my pregnancy chances suffer if embryos are frozen?
If you are suffering from early signs of OHS and have had a Buserelin trigger we will need to freeze all of your embryos as the lining of the womb will not develop properly to allow embryos to grow. For patients who are not symptomatic but for whom more than 20 eggs are collected at egg collection we still now advise that all embryos are frozen. This will not only reduce/eliminate your risks of developing significant OHS but also improve your overall chances of pregnancy. When we have looked at the results from fresh and frozen embryo replacement in patients with excessive response and more than 20 oocytes collected we have found that because of the increased stress on the lining of the womb with high levels of hormones when high egg numbers are retrieved, the chances of an individual embryo implanting and making a healthy pregnancy were more than double for every frozen embryo replaced.
Is there anything I should do?
Ensure that you do not become overly dehydrated. You should drink plenty of fluid. You should remain mobile but should take the opportunity to rest.
What happens about my embryo transfer?
Because of the benefit to improving pregnancy rates all embryos will be electively frozen at the blastocyst stage ( day 5 after collection). We then recommend that at least two periods occur before an embryo is defrosted and replaced. You will be seen after collection and the unit will wish to keep in touch to check for any symptoms you may be experiencing. You will be seen a few weeks after collection where the clinician will discuss the best method of treatment to prepare the womb for your embryo replacement. In very rare circumstances where embryos develop but are unsuitable for freezing a fresh transfer may be considered after very careful assessment and discussion with the clinician.
For more information about Frozen Embryo Transfer, visit our dedicated page.
What do I need to do now?
After egg collection you will be discharged with advice that will give you contact details for Northwest Fertility and Manchester fertility services . During the working week you can contact the fertility clinic to discuss any concerns.
The nurse from the fertility unit will advise you about any of your symptoms that may require further investigation. If a freeze-all cycle in response to OHS has been advised, the nurses will contact you regularly both to assess your symptoms and advise with regard to the development of embryos, as well as organising your follow up scans and appointments.



